Skin cancer awareness month - Understanding Melanoma Posted on 18 May 2023
How Common is Melanoma?
Did you know skin cancer is the most common form of cancer in the United States? There are three main forms of skin cancer: basal cell carcinoma, squamous cell carcinoma, and mela noma. Melanoma is the most serious form of skin cancer because of its ability to spread rapidly to other organs if not discovered early. It develops in our skin’s melanocytes, the cells that produce color in our skin. The rates of melanoma are increasing every year in the United States. Melanoma accounts for approximately 1% of skin cancers; however, it causes the majority of skin cancer deaths. The American Cancer Society estimates 106,110 cases of melanoma will be diagnosed in the United States in 2021. Approximately 7,180 of these cases will be fatal.
Who is at Highest Risk?
Melanoma is 20 times higher in whites than African Americans. According to the American Cancer Society, the lifetime risk of getting melanoma is 2.6% in Whites, 0.1% in Blacks, and 0.6% for Hispanics. Whites with red or blonde hair, blue or green eyes, and skin that freckles or burns easily are at the highest risk for melanoma. A history of one or more blistering sunburns increases one's risk for melanoma. Age is also a factor in melanoma. Most cases are diagnosed after the age of 65; however, rates of melanoma are increasing in younger individuals. In fact, it is one of the most common cancers diagnosed in young women. It is more common in men after the age of 50; however, women are more likely to be diagnosed before age 50. Your risk also increases if you've had a family member with melanoma. This can be due to shared environmental experiences (i.e., more exposure to UV light) and/or genetic predisposition. Individuals with a weakened immune system, such as those with HIV or a history of organ transplant, are also at a higher risk for melanoma.
What Causes Melanoma?
Over 90% of melanomas are caused by UV light, including indoor tan ning beds and outdoor sun exposure. On more rare occasions, melanoma can be caused by a genetic mutation. It most commonly occurs on sun-ex posed areas of the body, such as the back, arms, legs, and face. The first signs of melanoma are a change in an existing mole or the development of a new, pigmented lesion on your skin. Some 20-30% of melanomas arise in existing moles, while 70-80% occur in newly-appearing lesions.
What Are the Tools for Detecting Melanoma?
The most important aspect of mel anoma treatment is early detection. Knowing your own skin is critical! Inspect your skin and become familiar with your freckles, moles, and marks so you are aware if anything changes. If you can find a melanoma early, the chances of survival increase drastically. There are several points to evaluate when checking a mole for irregularity. In dermatology, we often refer to the ABCDE's of melanoma when evaluating pigmented lesions:
Asymmetry Melanoma is often asymmetric, unlike benign moles
Border Melanoma often has ill-defined borders
Color Melanoma lesions typically have more than one color
Diameter Melanoma is usually larger than 5mm, the diameter of a pencil eraser
Evolving Melanoma often changes its characteristics, such as size, shape, and color, unlike benign moles that do not frequently evolve
Cancerous moles vary greatly in appearance, including one or more of the above criteria. Additionally, it is important to see a dermatology provider on a yearly basis for a thorough skin check. In between visits to the dermatologist, make sure to check your skin every month, including the bottoms of the feet and in between the toes. These are hidden areas where melanoma may occur and people often forget to check. Melanomas are more likely to occur in hidden areas in people with a higher Fitzpatrick skin type. The following melanomas may also be found in hidden areas:
Acral-‐Lentiginous Melanoma is Rare form of melanoma occurring underneath a toenail or fingernail. This is more likely to occur in Asians and people with higher Fitzpatrick skin color classification.
Melanoma of the Mucous Mem branes Includes the digestive tract, urinary tract, vagina, and oral mucosa. These are more difficult to detect as they can mimic more common conditions.
Melanoma in the Eye Melanoma in the eye is most likely to occur in the uvea (the layer behind the white sclera).
In order to check for hidden melanomas, it is important to have a yearly eye exam with an ophthalmologist. Women should also see a gynecologist yearly to rule out moles or lesions in the genital areas.
How is Melanoma Diagnosed?
A thorough physical exam with a dermatology provider will be done. If an unusual lesion is detected, a sample (biopsy) will be removed and sent to a dermatopathologist for examination.
The type of sample will be determined by the dermatology provider and may include a punch biopsy or an excision al biopsy. The punch biopsy is done with a circular blade to remove the suspicious mole. An excisional biopsy will remove the lesion and a margin of normal tissue surrounding it. After melanoma is diagnosed, the next step is to stage the cancer. In order to stage the melanoma, the provider will look at the thickness of the melanoma, see if it has spread to lymph nodes, and look for possible metastases to other parts of the body. Increased thickness, positive lymph node involvement, and metastases to other parts of the body will all increase the severity of the melanoma.
How is Melanoma Treated?
Early-stage melanoma may be treated with surgery alone; however, more advanced stages may require other treatments. Based on the stage of melanoma, treatment may include immunotherapy, radiation, chemotherapy, or targeted therapy drugs specifically for melanoma. Several factors go into making a treatment plan. The dermatologic oncology gy team will consider age, overall health, location of melanoma, stage of melanoma, and the likelihood of cure. Clinical trials in melanoma are common in academic institutions and may be offered as part of the overall treatment plan. The following are treatments for melanoma that has spread beyond the skin:
Radiation Therapy This type of therapy uses high-‐powered energy beams to kill cancer cells. This can be used to treat cancers not able to be fully removed by surgery.
Chemotherapy Chemotherapy uses drugs specified to kill cancer. This can be given in pill or intravenous form.
What Are Some Tools for Preventing Melanoma?
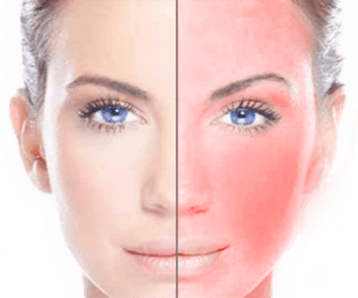
There is no such thing as a healthy tan. Change in skin color pigment indicates damage to the skin cells, which may lead to skin cancers, including melanoma.
Avoiding UV light is the best way to protect yourself from melanoma. Another important tool for melanoma prevention is wearing sun protection daily.
Consistency is key! Apply SPF 30, preferably a mineral-‐based sunblock, to sun-exposed areas every morning. If you are going to be in the sun for a prolonged period of time, it's important to reapply sunblock every two hours. Sun-protective clothing is also a great option to pair with sunblock. Sunglasses that block UVA and UVB light are important to protect the eyes. Do not forget to protect the scalp, ears, and nose, which are commonly forgotten areas where we see a lot of sun damage.
Additionally, it is important to avoid direct sunlight as best you can, particularly the peak sun hours between 10 AM 2 PM. Seek shade whenever possible.